Chronic pain: always prescribe gabapentin
"You always have to think about it, even though you don't want to. Chronic pain is very penetrating, like a police siren, or pneumatic drill. Nothing seems to help it - often not even more ibuprofen."
That’s the sort of thing you hear in the consulting room at the Doctors’. Does this also apply to dogs? One might think so, when you see how veterinarians prescribe gabapentin, triptans and other centrally acting painkillers for so-called "chronic pain patients". Especially the use of gabapentin for arthrosis is very popular with vets, but it is absolutely wrong and in no way achieves the desired results in pain therapy. Gabapentin is effective for neuropathic pain, but arthrosis is not a neuropathic pain. The effect of this medication is to make the dog calmer. This idea or this misuse of these medications can have fatal consequences, among other things, as our example from my practice today will show you.
In dogs, unfortunately, chronic is confused with long-lasting pain. The result of this is an increased use of these neuroleptics for so-called pain patients. You may now think, what is the difference here? It is quite significant. It is precisely a long-lasting pain that becomes chronic. This means that other parts of the body, especially in the musculoskeletal system, are affected. This leads to overloading or relieving, and thus radiates to the entire musculoskeletal system.
Acute pain
We all know acute pain. We hit our head on a low roof beam, or we shut our finger in a door, or hit it with a hammer. This list is almost endless. This is the same with a dog. He is bumped by another dog and does a somersault, or he jams his paw in the cattle grid. This hurts, the dog yelps and limps. There is no question that this is an acute pain situation. Either you can treat your dog yourself, or you can go to the vet. An adequate therapy will be initiated, and in a few days the worst will be over.
Chronic pain
Exclusively time-related definition for pain with an uninterrupted duration of pain of at least six months. In dogs, this can also refer to the period of 3 – 6 months.
Chronic pain is a pain with consequences/impairment on somatic, psychological and social levels. In dogs this means, in the case of long-lasting pain in the back, for example a slipped disc or transitional vertebrae, that the movement becomes adapted. This means that the dog has too little thrust in the hindquarters and compensates for this with a pull-move of the forehand. The shoulders now perform statics and dynamics in one. This is the sort of case I see daily in the practice.
The psychological aspect of chronic pain in the dog can cause fear or aggression, or both, especially depending on the breed. For example, in a Ridgeback, this often not only causes fear but unfortunately also aggression. The aggressive aspect should not be underestimated, as depending on size, and sex of the dog this could have very serious consequences.
By the social component, for example, we refer to the fact that the dog may become withdrawn, apathetic/listless or sleepy. These belong to the category of a drop in performance. This is often the first effect that an owner consciously notices in connection with a pain patient, but he is unaware of the reason. It is frequently attributed to old age, or much worse, hypothyroidism. If this is not confirmed, the listlessness remains puzzling to the owner. Often at this point, patients are presented to my practice.
Pain memory
This term is often misunderstood and placed in the context of chronic. It refers to central nervous, functional and morphological reactions to pain stimuli. These are therefore central nervous reactions and circuits in the brain, especially when the peripheral pain stimuli are no longer present, these pain impulses continue to fire in the brain. In short; "pain out of control".
Neuropathic pain
Neuropathic pain is a proven or suspected functional disorder or pathological change in one or more nerves (mononeuropathy or polyneuropathy). A good example in dogs is the intervertebral disc problem with a nerve root disease (radiculoneuritis or tumour in the brachial plexus (nerve node under the armpit)).
Arthrosis/arthritic pain
Osteoarthritis is a degenerative process of one or more joints. It is a mechanical and inflammatory process with marked functional limitations. The functional part of this pathology is very important. This is also the reason why patients with osteoarthritis at best show practically no lameness and/or pain if the joint is still functionally partially intact. Functional means that the joint can no longer move in the anatomically prescribed path due to the degeneration, respectively moves only within the bounds of possibility. This depends on the severity of the arthrosis.
When assessing the level of pain in osteoarthritis, a distinction must be made between pain on movement versus pain at rest, or worse, pain while lying down. Dogs in the last category change sleeping places very often, especially at night, are restless and pant a lot, thus robbing the owner of sleep. A vicious circle that also affects the owner and can cause emotions to run high. This in turn leads to the patient's presentation to the orthopaedic vet.
Example from the practice
Our patient today is an 8-year-old sighthound. He was vaccinated in November. Up to the time of the vaccination, the patient was healthy. He had been regularly wormed and also vaccinated annually. At that time, nothing indicated what was about to happen. Shortly before Christmas the patient became very unwell, had difficulty with the hindquarters, especially when walking, and suffered a loss of strength in the hindquarters, pain in the spine as well as reddening of the paws. First in both front paws, then all 4 paws. The owner went to the vet, and had the dog examined. As the proprioception in the hindquarters was slowed down, a neurological process was suspected. Gabapentin was then administered. A few hours after the administration of gabapentin, the dog became paralysed in all four limbs, a tetraparesis. As this paralysis was completely unexpected, the dog was referred to a neurologist. Further investigations, neurological expertise, laboratory examination as well as an MRI were performed.
There were no indications or results that would explain and confirm the clinical picture. All laboratory results were also unremarkable.
Gabapentin was continued. In addition, antibiotics and Prednisolone were given. There was no improvement in the short term, and only when the gabapentin was stopped did the tetraparesis slowly disappear. The cortisone and antibiotics were continued. MRI findings were obtained but these could not with certainty account for the dog's existing clinical symptoms.
MRI findings:
Focal V-shaped lesion / myelopathy of the dorsal funiculus at the level of C3-4 - Differential diagnoses: degenerative changes such as gliosis, focal myelitis, sensory neuronopathy. Mild to moderate degeneration of intervertebral discs C3-7 with minimal production without compression of the spinal cord. Morphologically unremarkable brain.
Comments: The clinical relevance of the V-shaped lesion at the level of C3-4 is questionable. However, ganglioradiculitis (sensory neuronopathy) cannot be excluded and could explain part of the symptoms. Unfortunately, a definitive diagnosis can only be made histologically.
Functional orthopaedic examination
The patient is walking in a right lateral stance and shows a distinct ataxic movement in the hindquarters. There is asymmetry in the pelvis and varus in the left elbow. Given the former paralysis, the level of movement is surprisingly good, but still falls short of what we’d call normal movement. The head posture is tilted to the right, and shows atrophy regression of the temporalis muscles as well as the masseter on the right side; cervical spine is bent laterally on the right side, and the ROM of the cervical spine shows clear restrictions, especially on the right side.
Functional differences can also be seen in the right shoulder and right elbow. The varus position in the left elbow is the result of the load transfer from the right side.
Graphic of the functional examination (kinematics)
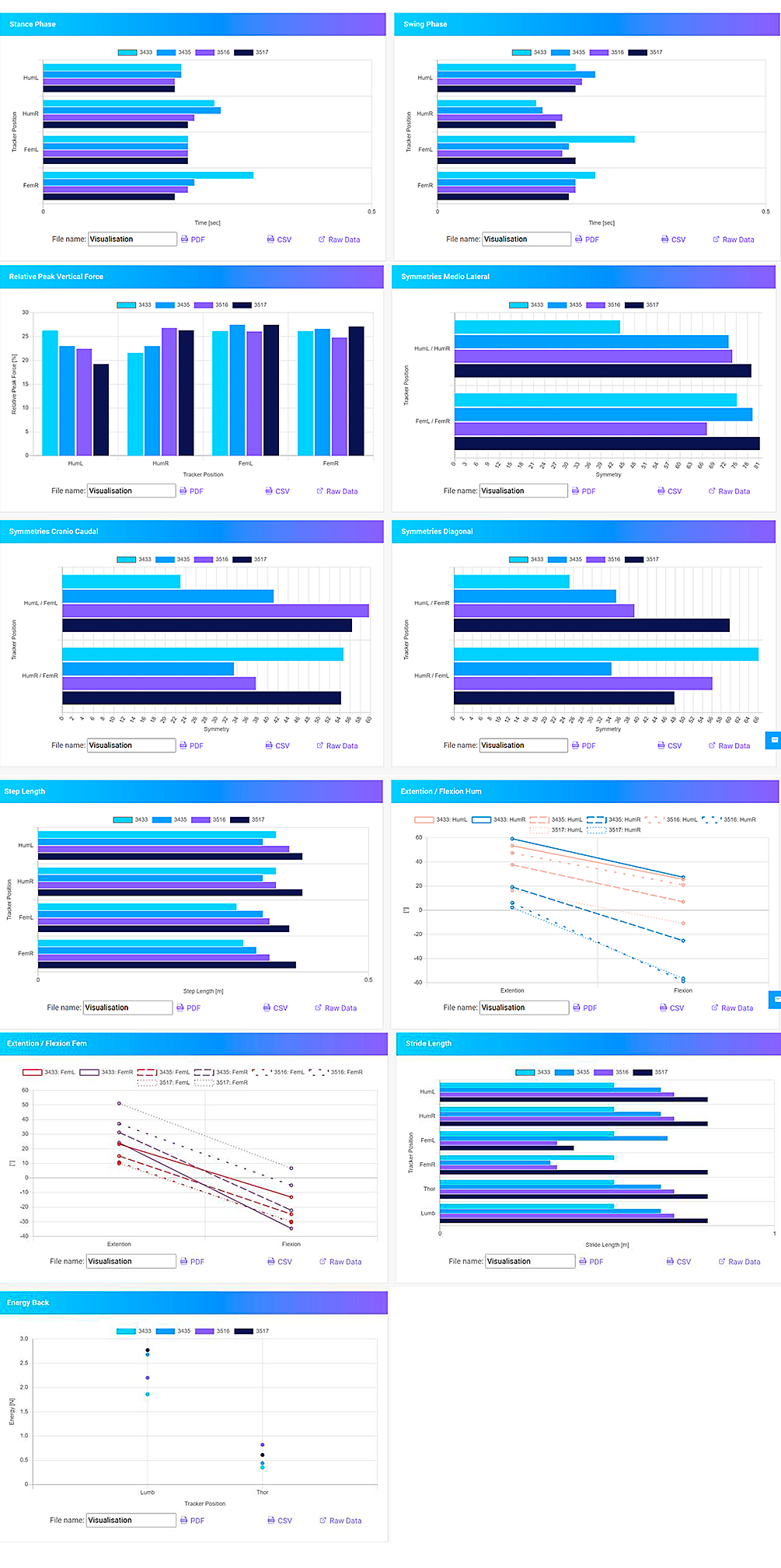
After the functional orthopaedic examination, the patient received orthopaedic manual, kinematically controlled treatment. The light blue bars are the results before the orthopaedic treatment, the dark blue ones are the results immediately after.
The purple bars show the movement analysis on the occasion of the control visit 3 weeks later, following which the patient received a second orthopaedic manual kinematically controlled treatment, focussed in particular on one hand on the cervical spine, and on the other on the head, more precisely at the motor coordination in the cerebrum, the right frontal lobe. The black values are the results of the analysis after this second treatment, and as can be seen, the results are very positive.
Conclusion: through the orthopaedic kinematic examination and treatment, it can be stated that the changes in the cervical spine had a clinical relevance. However, this was first triggered by a mechanical blunt traumatic event. This was successfully resolved by the two functional orthopaedic treatments. Now the rehabilitation and regeneration phases begin. This will be achieved through regular aqua-therapy.
The consequences of therapy with gabapentin
As is unfortunately evident from this example, the fact is that veterinarians repeatedly use gabapentin immediately in the case of neurological findings. This is very frequently based on a faulty generalisation: Neurological deficit equals therapy with gabapentin. Whether or not a functional disturbance of nerves is present, or whether this is painful, is not the subject of the question. It would certainly be desirable for this to be further differentiated. It is thus obvious that the use of gabapentin needs to be more carefully considered.
It should also be noted that this medication is not equally well tolerated in all breeds and individuals. Especially in sight-hounds, the use of gabapentin needs really careful consideration. The positive therapeutic successes need to be weighed against the potential (negative) side effects, in order to judge what seems to make best sense as a therapy. This is also my personal point of view as an owner of sight-hounds and as a veterinarian.
Another aspect is the use of gabapentin for arthrosis. The arthrosis does not show any neuropathic pain and therefore the therapy with gabapentin in arthrosis is an absolute false indication for the use of this drug. There needs to be an urgent rethink among veterinarians, about this point. 10 years ago, I tried to develop a test for neurogenic inflammation in Rosenheim, Basel. At that time, existing possibilities for the detection of substance P as well as Calcitonin Gene Related Hormone were difficult. Nevertheless, we will soon be able to take a significant step in the treatment of osteoarthritis.
Osteoarthritis causes pain that is either clinically manifest at the onset of movement or during prolonged exercise. I already referred to this fact at the beginning.
It is a functional pain and above all a chronified pain with an incorrect and/or overloaded posture. It is precisely here that the functional diagnostics of movement analysis can be of great service in the future. Even the therapy of neurogenic inflammation will not change this in the future. If osteoarthritis is understood as a mechanical-inflammatory pain process and is also diagnosed and presented in this way, osteoarthritis therapy can really make progress.
The use of gabapentin for osteoarthritis has no effect because this pain is not neuropathic. The aim of the therapy is only to sedate the dog, so the dog is tired; the perception of pain is not reduced, only the activity is reduced. Thus, a goal is achieved, the dog no longer wants to move because it is tired. This means a drop in performance and, as a consequence, the owners again worry. Is this the goal of therapy? Every dog owner should answer this question for himself.
We will deal with the topic of arthrosis in one of the next newsletters and look at the causes and consequences as well as therapy options from different angles.
